Glasgow Coma Scale Pdf
Glasgow Coma Scale: While the 15-point scale is the predominant one in use, this is in fact a modification and is more correctly referred to as the Modified Glasgow Coma Scale. The original scale was a 14-point scale, omitting the category of 'abnormal flexion'. A Glasgow Coma Scale (GCS) assessment should be conducted on every patient. Background The GCS was developed at the University of Glasgow’s Institute of Neurological Sciences. It is numerical rating system, originally used for measuring conscious state following traumatic brain injury, which has become a widely used and recognised.
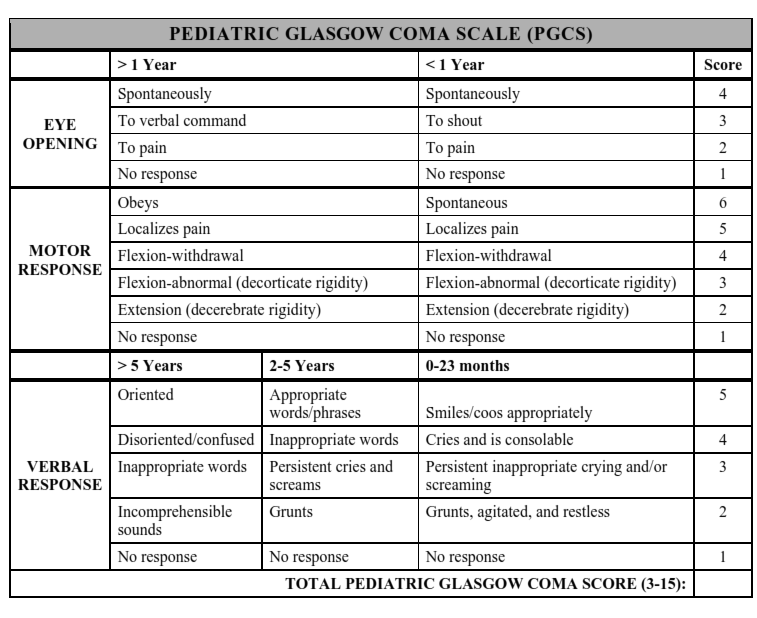
Paediatric Glasgow Coma Scale Pdf
| Glasgow Coma Scale | |
|---|---|
| Medical diagnostics | |
| MeSH | D015600 |
| LOINC | 35088-4 |
The Glasgow Coma Scale (GCS) is a neurologicalscale which aims to give a reliable and objective way of recording the state of a person's consciousness for initial as well as subsequent assessment. A person is assessed against the criteria of the scale, and the resulting points give a person's score between 3 (indicating deep unconsciousness) and either 14 (original scale) or 15 (more widely used modified or revised scale).
GCS was initially used to assess a person's level of consciousness after a head injury, and the scale is now used by emergency medical services, nurses, and physicians as being applicable to all acute medical and trauma patients. In hospitals, it is also used in monitoring patients in intensive care units.
The scale was published in 1974 by Graham Teasdale and Bryan J. Jennett, both professors of neurosurgery at the University of Glasgow's Institute of Neurological Sciences at the city's Southern General Hospital.
GCS is used as part of several ICU scoring systems, including APACHE II, SAPS II, and SOFA, to assess the status of the central nervous system. The initial indication for use of the GCS was serial assessments of people with traumatic brain injury[1] and coma for at least six hours in the neurosurgical ICU setting, though it is commonly used throughout hospital departments. The similar Rancho Los Amigos Scale, is used to assess the recovery of traumatic brain injury.
GCS was updated following a review of the helpfulness and usefulness of the scale from clinicians. It was decided that several things required updating, like the Eye Response element, meaning that instead of responding to 'Painful Stimuli' being regarded as a 2, a person that opens their eyes in response to pressure is now considered a 2 in the Eye Response element.[2]
- 1Elements of the scale
- 6References
Glasgow Coma Scale Pdf Chart
Elements of the scale[edit]
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| Eye | Does not open eyes | Opens eyes in response to pain | Opens eyes in response to voice | Opens eyes spontaneously | N/A | N/A |
| Verbal | Makes no sounds | Makes sounds | Words | Confused, disoriented | Oriented, converses normally | N/A |
| Motor | Makes no movements | Extension to painful stimuli (decerebrate response) | Abnormal flexion to painful stimuli (decorticate response) | Flexion / Withdrawal to painful stimuli | Localizes to painful stimuli | Obeys commands |
Note that a motor response in any limb is acceptable.[4]The scale is composed of three tests: eye, verbal and motor responses. The three values separately as well as their sum are considered. The lowest possible GCS (graded 1 in each element) is 3 (deep coma or death), while the highest is 15 (fully awake person).
Eye response (E)[edit]
There are four grades starting with the most severe:
- No opening of the eye
- Eye opening in response to pain stimulus. (a peripheral pain stimulus, such as squeezing the lunula area of the person's fingernail is more effective than a central stimulus such as a trapezius squeeze, due to a grimacing effect).[5]
- Eye opening to speech. (Not to be confused with the awakening of a sleeping person; such people receive a score of 4, not 3.)
- Eyes opening spontaneously
Verbal response (V)[edit]
There are five grades starting with the most severe:
- No verbal response
- Incomprehensible sounds. (Moaning but no words.)
- Inappropriate words. (Random or exclamatory articulated speech, but no conversational exchange. Speaks words but no sentences.)
- Confused. (The person responds to questions coherently but there is some disorientation and confusion.)
- Oriented. (Person responds coherently and appropriately to questions such as the person’s name and age, where they are and why, the year, month, etc.)
Motor response (M)[edit]
There are six grades:
- No motor response
- Decerebrate posturing accentuated by pain (extensor response: adduction of arm, internal rotation of shoulder, pronation of forearm and extension at elbow, flexion of wrist and fingers, leg extension, plantarflexion of foot)
- Decorticate posturing accentuated by pain (flexor response: internal rotation of shoulder, flexion of forearm and wrist with clenched fist, leg extension, plantarflexion of foot)
- Withdrawal from pain (absence of abnormal posturing; unable to lift hand past chin with supraorbital pain but does pull away when nailbed is pinched)
- Localizes to pain (purposeful movements towards painful stimuli; e.g., brings hand up beyond chin when supraorbital pressure applied)
- Obeys commands (the person does simple things as asked)
Interpretation[edit]
Individual elements as well as the sum of the score are important. Hence, the score is expressed in the form 'GCS 9 = E2 V4 M3 at 07:35'.
Generally, brain injury is classified as:
- Severe, GCS < 8–9
- Moderate, GCS 8 or 9–12 (controversial)[6]
- Minor, GCS ≥ 13.
Tracheal intubation and severe facial/eye swelling or damage make it impossible to test the verbal and eye responses. In these circumstances, the score is given as 1 with a modifier attached (e.g. 'E1c', where 'c' = closed, or 'V1t' where t = tube). Often the 1 is left out, so the scale reads Ec or Vt. A composite might be 'GCS 5tc'. This would mean, for example, eyes closed because of swelling = 1, intubated = 1, leaving a motor score of 3 for 'abnormal flexion'.
The GCS has limited applicability to children, especially below the age of 36 months (where the verbal performance of even a healthy child would be expected to be poor). Consequently, the Paediatric Glasgow Coma Scale was developed for assessing younger children.
Revisions[edit]
- Glasgow Coma Scale: While the 15-point scale is the predominant one in use, this is in fact a modification and is more correctly referred to as the Modified Glasgow Coma Scale. The original scale was a 14-point scale, omitting the category of 'abnormal flexion'. Some centres still use this older scale, but most (including the Glasgow unit where the original work was done) have adopted the modified one.
- The Rappaport Coma/Near Coma Scale made other changes.
- Meredith W., Rutledge R, Fakhry SM, EMery S, Kromhout-Schiro S have proposed calculating the verbal score based on the measurable eye and motor responses.
- The most widespread revision has been the Simplified Motor and Verbal Scales which shorten the respective sections of the GCS without loss of accuracy.[7]
- The GCS for intubated people is scored out of 10 as the verbal component falls away
Controversy[edit]
The GCS has come under pressure from some researchers who take issue with the scale's poor inter-rater reliability and lack of prognostic utility.[8] Although there is no agreed-upon alternative, newer scores such as the Simplified motor scale and FOUR score have also been developed as improvements to the GCS.[9] Although the inter-rater reliability of these newer scores has been slightly higher than that of the GCS, they have not gained consensus as replacements.[10]
VLC Media Player 2019 Windows 10VLC Media Player 2019 Windows 10 also can look for album covers. Vlc. This is particularly of use when you have saved a video in several components or just want to view a few shorter videos. A playlist purpose allows for numerous shows to perform one after the other.
See also[edit]
- AVPU scale
References[edit]
- ^Teasdale G, Jennett B (1974). 'Assessment of coma and impaired consciousness. A practical scale'. Lancet. 2 (7872): 81–4. doi:10.1016/S0140-6736(74)91639-0. PMID4136544.
- ^'What's new - Glasgow Coma Scale'. www.glasgowcomascale.org. Retrieved 2018-06-24.
- ^Russ Rowlett. 'Glasgow Coma Scale'. University of North Carolina at Chapel Hill.
- ^Hutchinson’s clinical methods 22nd edition
- ^Iankova, Andriana (2006). 'The Glasgow Coma Scale: clinical application in Emergency Departments'. Emergency Nurse. 14 (8): 30–5. doi:10.7748/en2006.12.14.8.30.c4221. PMID17212177.
- ^'Resources data'(PDF). www.cdc.gov.
- ^Gill M, Windemuth R, Steele R, Green SM (2005). 'A comparison of the Glasgow Coma Scale score to simplified alternative scores for the prediction of traumatic brain injury outcomes'. Ann Emerg Med. 45 (1): 37–42. doi:10.1016/j.annemergmed.2004.07.429. PMID15635308.
- ^Green S. M. (2011). 'Cheerio, Laddie! Bidding Farewell to the Glasgow Coma Scale'. Annals of Emergency Medicine. 58 (5): 427–430. doi:10.1016/j.annemergmed.2011.06.009. PMID21803447.
- ^Iver, VN; Mandrekar, JN; Danielson, RD; Zubkov, AY; Elmer, JL; Wijdicks, EF (2009). 'Validity of the FOUR score coma scale in the medical intensive care unit'. Mayo Clinic Proceedings. 84 (8): 694–701. doi:10.4065/84.8.694. PMC2719522. PMID19648386.
- ^Fischer, M; Rüegg, S; Czaplinski, A; Strohmeier, M; Lehmann, A; Tschan, F; Hunziker, PR; Marschcorresponding, SC (2010). 'Inter-rater reliability of the Full Outline of UnResponsiveness score and the Glasgow Coma Scale in critically ill patients: a prospective observational study'. Critical Care. 14 (2): R-64. doi:10.1186/cc8963. PMC2887186. PMID20398274.
Sources[edit]
- Teasdale G, Murray G, Parker L, Jennett B (1979). 'Adding up the Glasgow Coma Score'. Acta Neurochir Suppl (Wien). 28 (1): 13–6. doi:10.1007/978-3-7091-4088-8_2. ISBN978-3-7091-4090-1. PMID290137.
- Meredith W, Rutledge R, Fakhry SM, Emery S, Kromhout-Schiro S (1998). 'The conundrum of the Glasgow Coma Scale in intubated patients: a linear regression prediction of the Glasgow verbal score from the Glasgow eye and motor scores'. J Trauma. 44 (5): 839–44, discussion 844–5. doi:10.1097/00005373-199805000-00016. PMID9603086.